Palliative care is an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.
Addressing suffering involves taking care of issues beyond physical symptoms. Palliative care uses a team approach to support patients and their caregivers. This includes addressing practical needs and providing bereavement counselling. It offers a support system to help patients live as actively as possible until death.
Palliative care is explicitly recognized under the human right to health. It should be provided through person-centered and integrated health services that pay special attention to the specific needs and preferences of individuals.
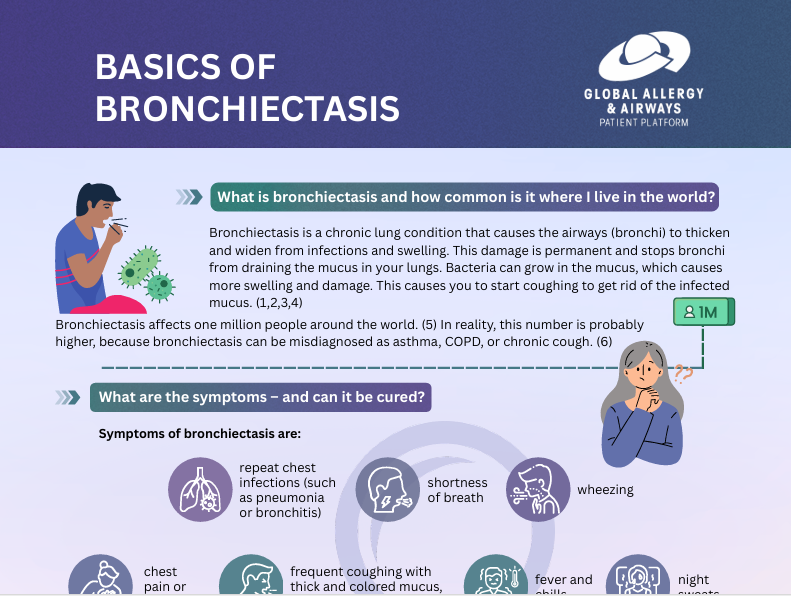
Palliative care is required for a wide range of diseases. The majority of adults in need of palliative care have chronic diseases such as cardiovascular diseases (38.5%), cancer (34%), chronic respiratory diseases (10.3%), AIDS (5.7%) and diabetes (4.6%). Many other conditions may require palliative care, including kidney failure, chronic liver disease, multiple sclerosis, Parkinson’s disease, rheumatoid arthritis, neurological disease, dementia, congenital anomalies and drug-resistant tuberculosis.
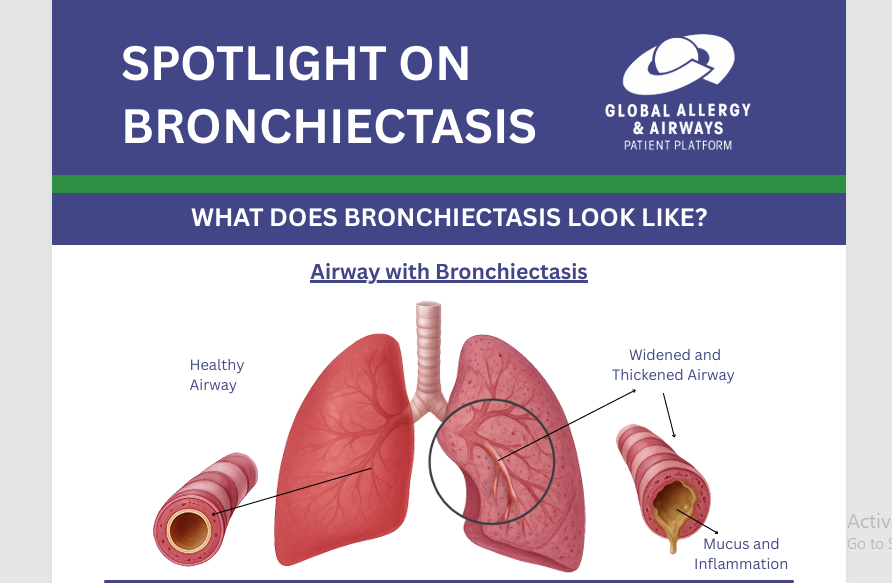
Pain and difficulty in breathing are two of the most frequent and serious symptoms experienced by patients in need of palliative care. For example, 80% of patients with AIDS or cancer, and 67% of patients with cardiovascular disease or chronic obstructive pulmonary disease will experience moderate to severe pain at the end of their lives. Opioids are essential for managing pain.
Opioids can also alleviate other common distressing physical symptoms including breathlessness. Controlling such symptoms at an early stage is an ethical duty to relieve suffering and to respect a person’s dignity.
Information presented on this page has been replicated from the linked WHO fact sheet. Please always refer to the original source on who.int for the latest version. Last update: March 2024.